Overview
Discectomy, a surgical procedure aimed at treating spinal disc herniation, stands as a cornerstone in the management of debilitating back pain and neurological symptoms. This minimally invasive intervention has revolutionized the field of spine surgery, offering relief to countless individuals suffering from the effects of herniated discs.
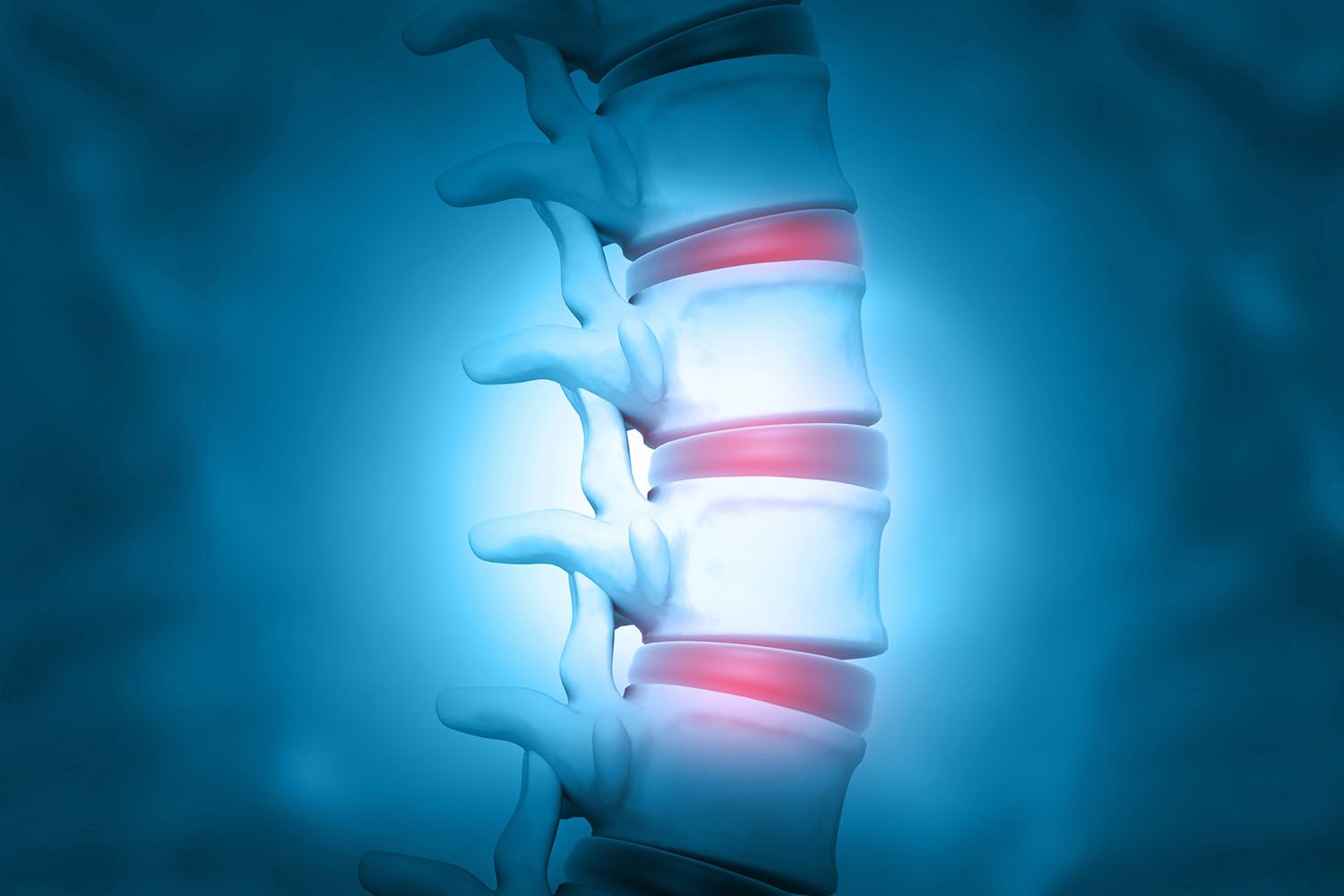
International research on discectomy has consistently demonstrated its efficacy in alleviating pain and restoring function in patients with symptomatic disc herniation. The procedure involves the removal of the protruding or ruptured portion of the intervertebral disc, thereby relieving pressure on adjacent nerves and reducing inflammation.
Studies have shown that discectomy not only provides immediate pain relief but also yields long-term benefits for patients, improving their quality of life and functional outcomes. Furthermore, advancements in surgical techniques and technology have led to reduced operative times, shorter hospital stays, and faster recovery periods, minimizing the disruption caused by traditional open surgeries.
The decision to undergo a discectomy is typically based on a thorough evaluation of the patient’s clinical presentation, imaging studies, and response to conservative treatments. While conservative measures such as physical therapy, medications, and epidural steroid injections may offer temporary relief, surgery becomes necessary for those who fail to find lasting improvement or experience progressive neurological deficits.
One of the key advantages of discectomy lies in its ability to target the underlying cause of symptoms while preserving spinal stability and function. By selectively removing the herniated disc material, surgeons can address the root cause of nerve compression without compromising the integrity of the spine.
Moreover, international guidelines and consensus statements endorse the use of discectomy as a safe and effective treatment option for carefully selected patients with symptomatic disc herniation. These recommendations underscore the importance of evidence-based practice and shared decision-making in optimizing patient outcomes and minimizing the risks associated with surgery.
While discectomy boasts high success rates and low complication rates, it’s essential to acknowledge that not all cases of disc herniation require surgical intervention. Patient selection, preoperative planning, and meticulous surgical technique are paramount in achieving favorable outcomes and reducing the likelihood of complications such as recurrent disc herniation or nerve injury.
Discectomy represents a valuable therapeutic option for individuals suffering from symptomatic disc herniation, offering the promise of pain relief and functional restoration. Through a combination of international research, evidence-based practice, and interdisciplinary collaboration, healthcare providers can deliver high-quality care to patients in need of surgical intervention for spinal disc herniation. By incorporating the latest advances in surgical technology and adhering to best practices, we can continue to improve outcomes and enhance the lives of individuals affected by this debilitating condition.



