Overview
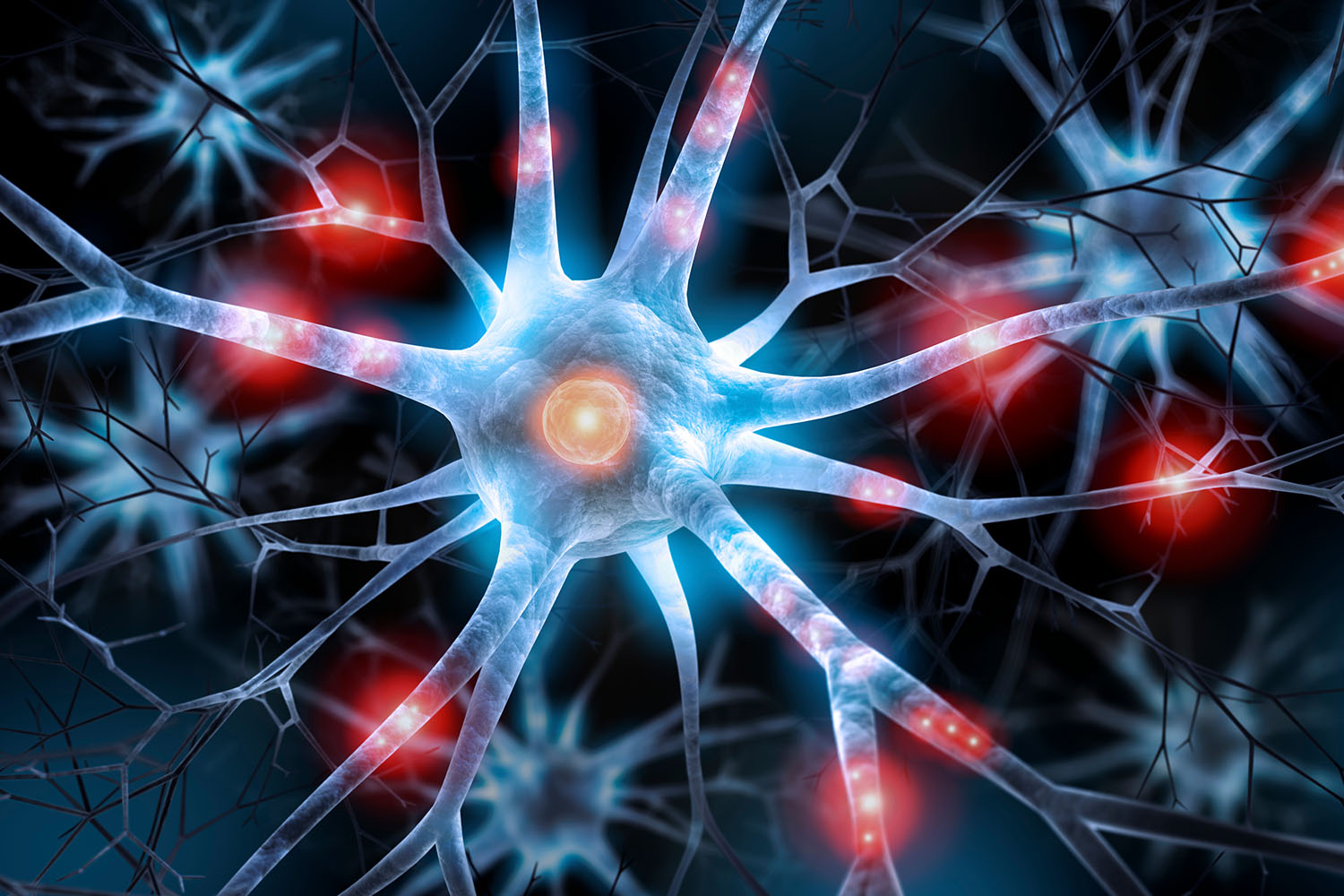
Nerve pain, clinically referred to as neuropathic pain, is a complex and often debilitating condition that affects millions of people worldwide. Unlike typical pain sensations, which arise from injuries or inflammation in tissues, nerve pain originates from dysfunction or damage to the nervous system itself. Delving into the realm of nerve pain reveals a fascinating yet challenging landscape shaped by scientific research and clinical observation.
The hallmark of nerve pain lies in its distinct characteristics, which can manifest as burning, stabbing, tingling, or electric shock-like sensations. These sensations, collectively termed neuropathic pain, can vary widely in intensity and frequency, often disrupting daily activities and significantly impacting quality of life.
Research into nerve pain has uncovered a multitude of factors contributing to its onset and persistence. Peripheral nerve damage resulting from conditions such as diabetes, autoimmune diseases, infections, or traumatic injuries can disrupt the normal transmission of signals within the nervous system, leading to aberrant pain sensations. Moreover, studies have elucidated the role of both peripheral and central sensitization in amplifying nerve pain signals, further complicating its management.
Peripheral sensitization involves changes in the peripheral nerves and tissues, leading to heightened sensitivity to pain stimuli. Meanwhile, central sensitization refers to alterations within the central nervous system, particularly in the spinal cord and brain, which amplify pain signals and contribute to the chronicity of nerve pain.
Understanding the multifaceted nature of nerve pain is crucial in developing effective treatment strategies. Medications targeting specific neurotransmitters or ion channels involved in pain transmission have shown promise in providing relief for some individuals. Additionally, therapies such as nerve blocks, spinal cord stimulation, and physical rehabilitation techniques offer alternative approaches to managing nerve pain and improving overall function.
However, treating nerve pain is not a one-size-fits-all endeavor. Each individual may respond differently to various treatment modalities, highlighting the importance of personalized care plans tailored to the unique needs of the patient. Moreover, addressing comorbid psychological factors such as anxiety and depression is essential, as they can exacerbate nerve pain symptoms and hinder recovery.
Nerve pain, or neuropathic pain, presents a complex clinical challenge that necessitates a multidisciplinary approach informed by research and clinical expertise. By integrating scientific insights with compassionate care, healthcare professionals can work towards alleviating the burden of nerve pain and restoring quality of life for individuals affected by this debilitating condition. Moreover, raising awareness about nerve pain and its impact can foster understanding and support within communities, ultimately empowering individuals to seek the help they need to manage their symptoms and reclaim their lives.



