Overview
In the ever-evolving landscape of pain management, one revolutionary approach shines brightly as a beacon of hope for individuals plagued by chronic pain: neuromodulation. This cutting-edge therapy offers a transformative solution by modulating the activity of the nervous system to alleviate pain and restore quality of life. Let’s delve into the depths of neuromodulation, exploring its mechanisms, benefits, and the research driving its efficacy.
Neuromodulation
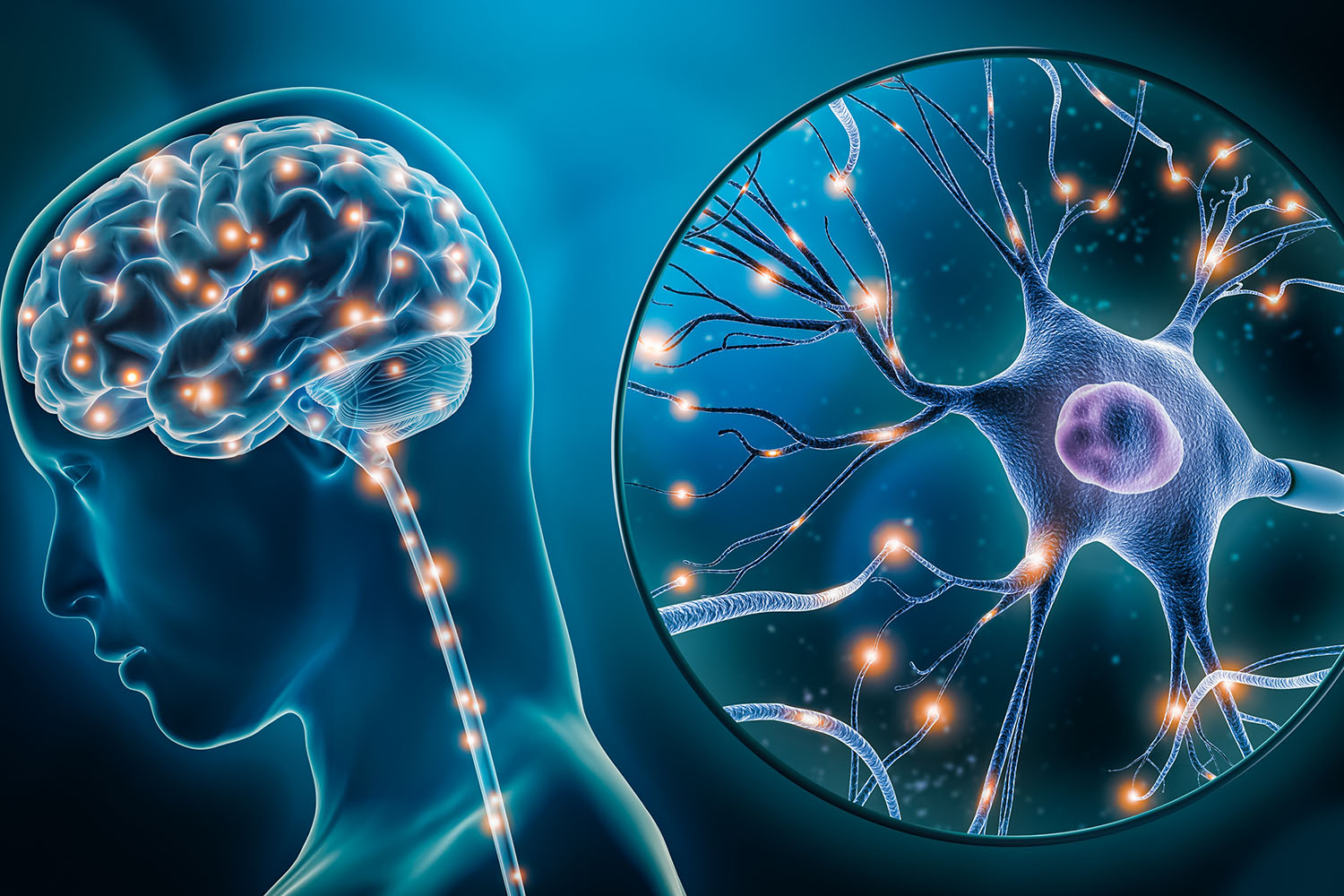
Neuromodulation : a term that reverberates with promise and possibility, symbolizing a paradigm shift in the treatment of chronic pain. But what exactly is neuromodulation, and how does it work? At its core, neuromodulation involves the targeted delivery of electrical or pharmaceutical agents to specific neural structures, altering their activity and interrupting the transmission of pain signals. This can be achieved through various modalities, including spinal cord stimulation, peripheral nerve stimulation, and deep brain stimulation, among others.
Research into neuromodulation has yielded compelling evidence of its efficacy across a wide spectrum of chronic pain conditions, ranging from neuropathic pain and failed back surgery syndrome to complex regional pain syndrome and refractory migraines. Numerous clinical trials and studies have demonstrated significant reductions in pain intensity, improvements in functional outcomes, and enhanced quality of life for patients undergoing neuromodulation therapy.
One of the most widely studied forms of neuromodulation is spinal cord stimulation (SCS), which involves the implantation of electrodes along the spinal cord to deliver electrical impulses that interfere with the perception of pain. Research indicates that SCS can provide long-term relief for individuals with chronic back and leg pain, often refractory to conventional treatments. Moreover, emerging evidence suggests that SCS may exert neuroprotective effects, potentially slowing the progression of chronic pain conditions and preventing central sensitization.
Peripheral nerve stimulation (PNS) represents another promising avenue in the realm of neuromodulation, offering targeted relief for localized pain syndromes such as neuropathies, peripheral nerve injuries, and post-amputation pain. Studies have shown that PNS can effectively alleviate pain, reduce medication reliance, and improve functional outcomes, particularly in cases where other therapies have proven ineffective or intolerable.
Deep brain stimulation (DBS), originally developed for the treatment of movement disorders such as Parkinson’s disease and essential tremor, has also emerged as a promising modality for certain chronic pain conditions. Research suggests that DBS may modulate pain-related neural circuits within the brain, offering relief for individuals with refractory neuropathic pain, trigeminal neuralgia, and other centralized pain syndromes.
As our understanding of neuromodulation continues to deepen and evolve, so too does its potential to revolutionize the field of pain management. With ongoing research driving innovation and refinement, the future holds promise for further advancements in neuromodulation therapies, offering renewed hope to millions of individuals worldwide grappling with the burdens of chronic pain. In the relentless pursuit of relief, neuromodulation stands as a testament to the remarkable progress achieved when science, compassion, and innovation converge in the service of healing.



