Overview
Rotator cuff surgery stands as a beacon of hope for individuals grappling with debilitating shoulder pain and limited mobility. Whether caused by acute injury or chronic wear and tear, rotator cuff tears can significantly impair daily activities and diminish quality of life. In this exploration, we delve into the intricacies of rotator cuff surgery, drawing upon research and facts to illuminate the journey from diagnosis to rehabilitation.
Diagnosis is the crucial first step on the path to rotator cuff surgery. Advanced imaging techniques such as magnetic resonance imaging (MRI) and ultrasound enable clinicians to visualize the extent and location of the tear with precision. Research underscores the importance of accurate diagnosis in guiding treatment decisions, ensuring optimal outcomes for patients undergoing rotator cuff surgery.
Once diagnosed, the decision to pursue surgery hinges upon various factors, including the size of the tear, the patient’s level of pain and functional impairment, and their overall health status. While smaller tears may respond well to conservative treatments such as physical therapy and corticosteroid injections, larger or symptomatic tears often necessitate surgical intervention to restore shoulder function and alleviate pain.
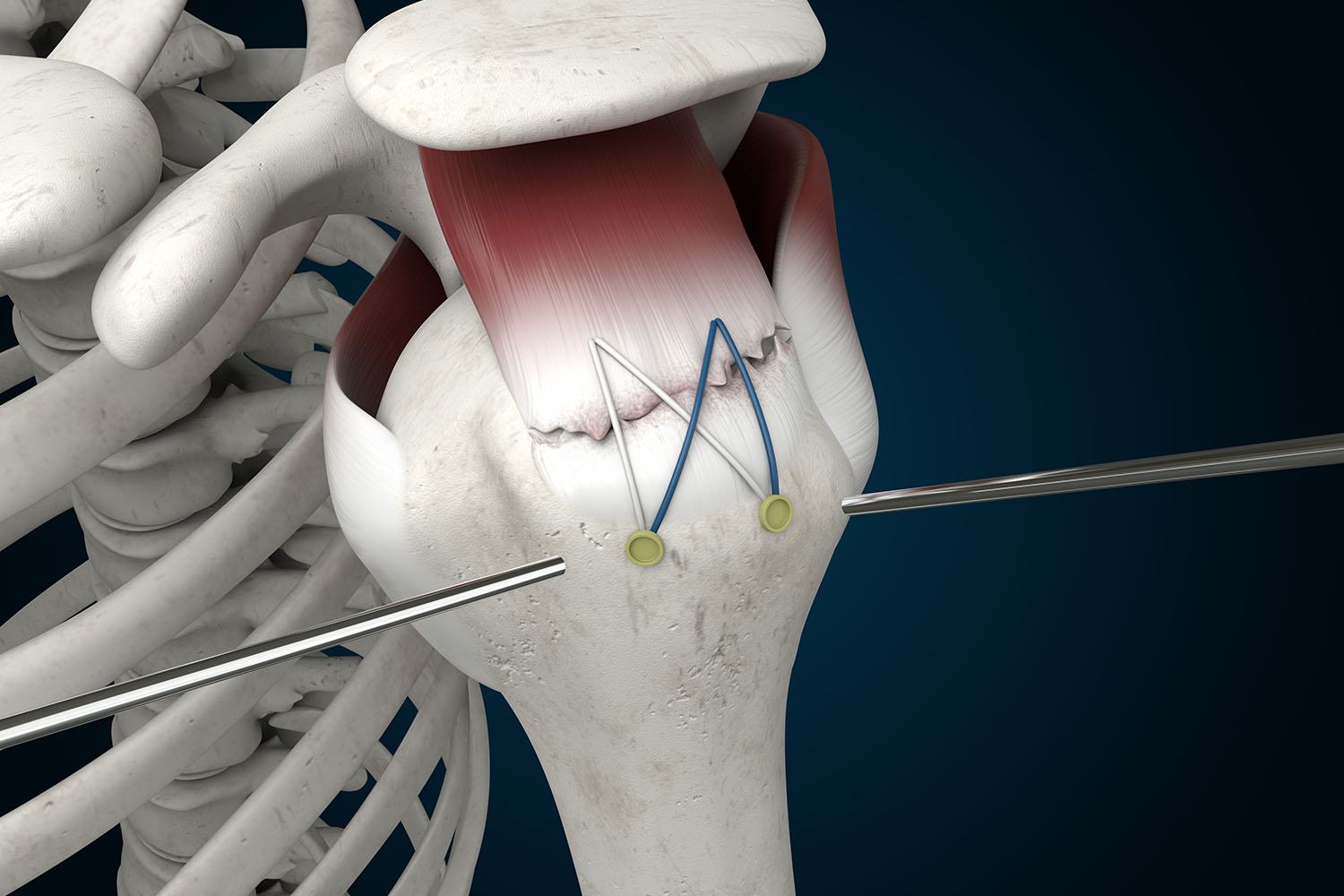
Rotator cuff surgery encompasses a spectrum of techniques tailored to the specific characteristics of the tear and the patient’s individual needs. Research has elucidated the efficacy of various surgical approaches, from arthroscopic repair, which involves small incisions and specialized instruments for minimally invasive repair, to open surgery for more extensive tears requiring direct visualization and access to the affected tissues.
During the surgical procedure, the torn tendon is meticulously reattached to its anatomical position on the humerus bone using sutures or anchors. Research advancements have led to innovations in surgical techniques and materials, optimizing tendon-to-bone healing and reducing the risk of re-tears postoperatively.
Rehabilitation following rotator cuff surgery plays a pivotal role in promoting recovery and restoring shoulder function. Research-based rehabilitation protocols emphasize gradual strengthening exercises, range of motion activities, and functional training to facilitate tissue healing and prevent stiffness or muscle atrophy. Adherence to prescribed rehabilitation regimens is paramount, as it directly correlates with long-term outcomes and functional recovery.
It’s essential to recognize that the road to full recovery following rotator cuff surgery may be challenging and require patience and perseverance. While surgical intervention offers the potential for significant improvement in symptoms and function, rehabilitation outcomes can vary depending on individual factors such as age, pre-existing health conditions, and adherence to postoperative care guidelines.
Rotator cuff surgery represents a cornerstone in the management of rotator cuff tears, offering renewed hope and restored mobility to countless individuals worldwide. By integrating research-driven approaches with personalized care, healthcare providers can guide patients through the surgical journey with confidence and compassion. Through continued advancements in surgical techniques, rehabilitation strategies, and patient education, the outlook for individuals undergoing rotator cuff surgery continues to brighten, paving the way for enhanced outcomes and improved quality of life.



